Welcome to COM’on the Society for Cardiovascular Pathology Case of the Month. Every month or so we will post a new COM’on and we invite everyone to give us their best diagnosis. If you follow SCVP on Twitter, we will send out a tweet each time a new COM’on has been posted.
Have a case you’d like us to use for a COM’on? Contact the SCVP Webmaster and let us know.
Case #78 – A 33-Year-Old Man With An Incidental Heart Mass
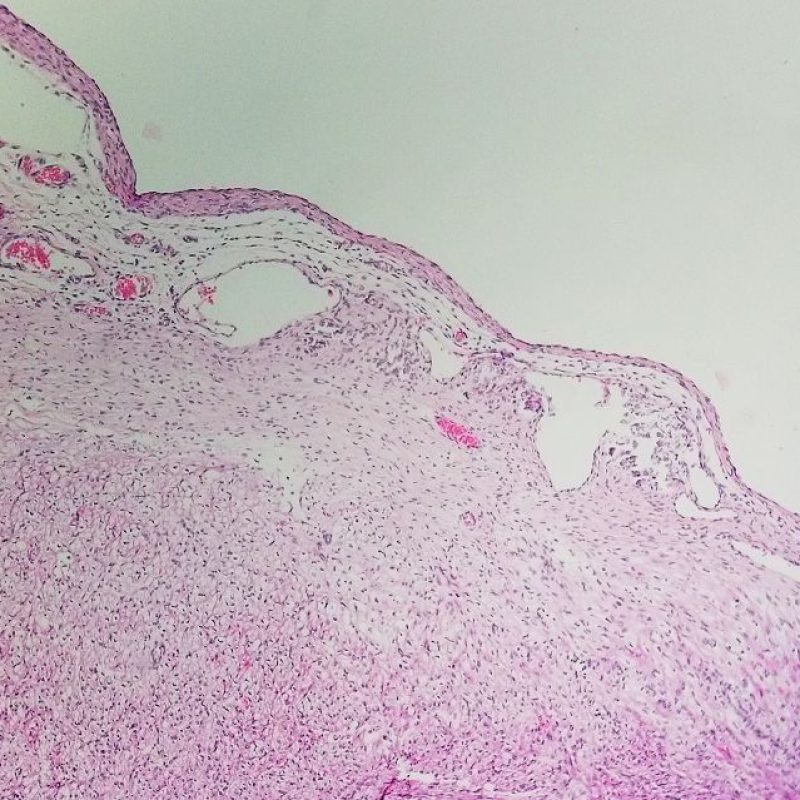
Cardiac varices are rare, endocardial structures characterized by blood-filled cysts lined with endothelial cells and containing organizing thrombus. Predominantly found in the right atrium, specifically at the posteroinferior border of the limbus of the fossa ovalis, these varices typically arise from dilated, thrombosed Thebesian veins and are frequently associated with phleboliths. The genesis of these formations may be linked to the embryonic integration of remnants from the left venous valve into the right side of the atrial septum.The reported incidence of cardiac varices is 0.07%. These varices are commonly asymptomatic and are typically discovered incidentally through imaging, during surgical inspections, or post-mortem examination.Varices manifest as elevated red-blue nodules, usually situated on the inferior limbus of the fossa ovalis. While their diameter typically remains below 20 mm, there are occasional instances where varices grow large enough to obstruct valvular orifices. Notably, these varices can be mistaken for cardiac myxomas.Histologically, varices exhibit dilated veins containing thrombus with variable organization. The venous media appears thinned, creating the appearance of endocardium-lined cysts. However, a thorough examination usually reveals areas where the venous media can be discerned (figure).Surgical intervention for cardiac varices remains uncertain, especially in asymptomatic cases.Cardiac Varix. Large, dilated vein containing blood. Note the vein wall on Movat stain.- Celeste Santos Martins, MD- Alison Krywanczyk, MD, FASCPReferencesRose AG. Venous malformations of the heart. Arch Pathol Lab Med. 1979 Jan;103(1):18-20. PMID: 153124.Maleszewski J, Burke A, Venoit J, Edwards W. AFIP Atlases of Tumor and Non-Tumor Pathology. Fifth series. Fascicle 17: Disorders of the heart and blood vessels. American Registry of Pathology; 2023.Shiraishi M, Kimura C, Yamaguchi A, Adachi H. Cardiac varix in the right atrium. Interact Cardiovasc Thorac Surg. 2012 May;14(5):686-8. doi: 10.1093/icvts/ivs015. Epub 2012 Feb 7. PMID: 22314009; PMCID: PMC3329297.
Case #77
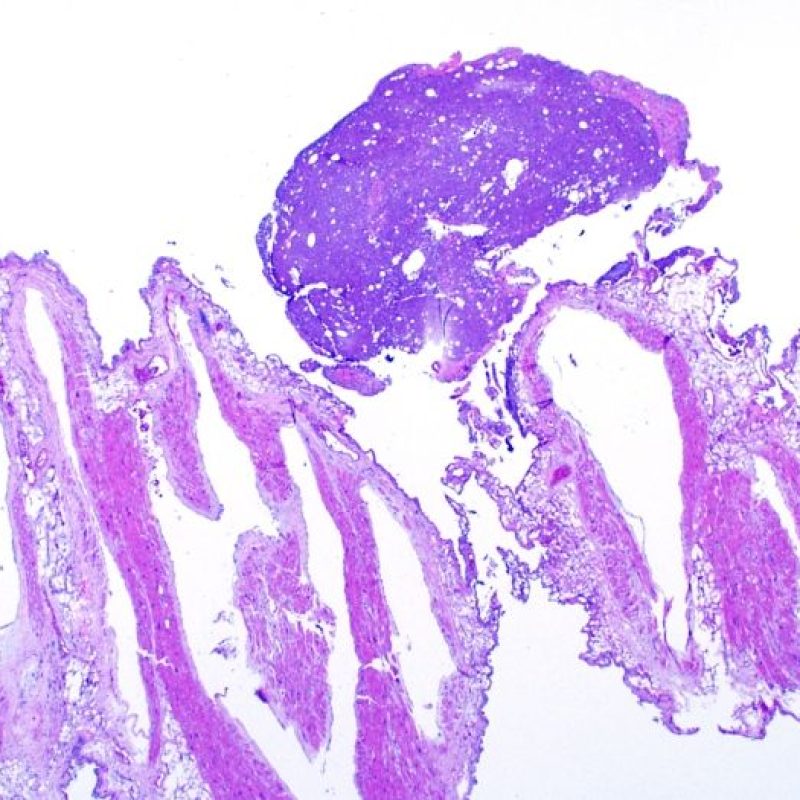
Unicuspid aortic valve (UAV) is a rare condition found in a very small percentage of patients undergoing echocardiography (~0.02%), but it is more common in those undergoing surgery for “pure aortic stenosis” (4-6%).There are two forms of UAV:Acommissural, where there is no attachment to the aortic wall at the orifice level. This abnormal valve is stenotic from birth, especially the acommissural variant, leading to symptoms appearing earlier than in those with bicuspid valves, even during the neonatal period.Unicommissural, where there is a single point of attachment to the aortic wall (see question image). In adults, unicuspid valves are primarily unicommissural. The free edge of the aortic cusp originates from a single aortic attachment, encircles the entire orifice, and returns near its original attachment, resulting in a relatively larger effective orifice area, forming an exclamation mark (!) or sometimes a “U” shape. Early valvular incompetence and associated cuspal trauma lead to secondary fibrosis and calcification. The raphe may be single or in two numbers, and sometimes none may be identified. Distances between true and false commissures, when present, are usually equal, dividing the valve into thirds.Nearly half (48%) of adult UAV patients coexist with ascending aortic dilatation, which may be caused by a synergistic effect of hemodynamic stress and a congenitally inherited weakness of the aortic media. Moreover, UAV patients have a higher risk of aortic dissection.Unicommissural UAV: Note the “U”-shaped configuration of the aortic orifice and a single point of attachment to the aortic wall (*). Encircled are 2 raphes, dividing the valve into thirds.- Celeste Santos Martins, MDReferencesYuan SM, Jing H, Lavee J. The unicuspid aortic valve. Cardiovasc J Afr. 2010 Mar-Apr;21(2):113-4. PMID: 20532437; PMCID: PMC5566075.Pan J. Unicuspid Aortic Valve: A Rare Congenital Anomaly. Cardiology. 2022;147(2):207-215. doi: 10.1159/000521623. Epub 2021 Dec 29. PMID: 34965530.Buja, L. Maximilian, and Jagdish Butany, eds. Cardiovascular Pathology. Fifth edition, Academic Press, 2022, London, England.
Case #76
WATCHMAN DEVICEAtrial fibrillation (AF) is associated with increased mortality and morbidity, with ischemic stroke being a significant complication. Thromboembolic cerebral ischemic stroke in AF patients can result from the formation and embolization of atrial thrombi, primarily originating from the left atrial appendage (LAA). To address this, various percutaneous devices, including the WATCHMAN Left Atrial Appendage System, have been introduced for LAA closure (LAAC). The WATCHMAN device (WMD) serves as an alternative to vitamin K antagonist therapy for stroke prevention in AF patients.The WMD consists of a self-expanding nitinol frame structure (1) with fixation barbs (2) and a permeable polyester fabric (3) covering its left atrial-facing surface.Available in diameters ranging from 21 to 33 mm to accommodate LAA size variations, the device is implanted using a catheter-based delivery system under local or general anesthesia. Fluoroscopic, angiographic, and ultrasound guidance is employed for optimal positioning, typically at or slightly distal to the ostium of the LAA via a transseptal approach.LAAC with the WMD is recognized as a secure and effective alternative to vitamin K antagonist therapy based on existing literature. According to current guidelines, LAAC is recommended primarily for AF patients with contraindications to long-term anticoagulant treatment (Class IIb). Nonetheless, several challenges have surfaced. Following LAAC, a vulnerable period emerges during the endothelialization of the WMD, heightening the risk of Device-Related Thrombus (DRT). The ideal duration for post-procedural anticoagulation therapy remains uncertain, and comprehensive studies comparing LAAC to novel oral anticoagulants are still lacking. Addressing these lingering questions requires additional randomized controlled trials, paving the way for a more definitive understanding of the role of LAAC in stroke prevention for patients with AF.- Celeste Santos Martins, MDReferencesFountain RB, Holmes DR, Chandrasekaran K, Packer D, Asirvatham S, Van Tassel R, Turi Z. The PROTECT AF (WATCHMAN Left Atrial Appendage System for Embolic PROTECTion in Patients with Atrial Fibrillation) trial. Am Heart J. 2006 May;151(5):956-61. doi: 10.1016/j.ahj.2006.02.005. PMID: 16644311.Stöllberger C, Schneider B, Finsterer J. WATCHMAN: an effective protection against stroke? Am Heart J. 2006 Oct;152(4):e35; author reply e37-8. doi: 10.1016/j.ahj.2006.04.038. PMID: 16996816.Wintgens LIS, Maarse M, Swaans MJ, Rensing BJWM, Van Dijk VF, Boersma LVA. The WATCHMAN left atrial appendage closure device for patients with atrial fibrillation: current status and future perspectives. Expert Rev Med Devices. 2020 Jul;17(7):615-626. doi: 10.1080/17434440.2020.1781615. Epub 2020 Jul 27. PMID: 32543911.January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society in Collaboration With the Society of Thoracic Surgeons. Circulation. 2019 Jul 9;140(2):e125-e151. doi: 10.1161/CIR.0000000000000665. Epub 2019 Jan 28. Erratum in: Circulation. 2019 Aug 6;140(6):e285. PMID: 30686041.
Case #75
MESOTHELIAL/MONOCYTIC INCIDENTAL CARDIAC EXCRESCENCE (MICE)Mesothelial/Monocytic Incidental Cardiac Excrescence (MICE) is a rare benign lesion typically identified during cardiac surgery. They have been described as nodules in the pericardium, or as a loose material in the pericardial fluid. Occasionally, they are submitted to the pathology laboratory as a “thrombus.” At gross examination, these excrescences are described as small fragments of tissue (measuring from <1 mm up to 3 cm), which vary in color from gray-white to brown or dark red.Microscopically, two cell populations are identified. The first population is represented by plump histiocytes with pale pink cytoplasm and prominent nuclear grooves. Immunohistochemistry studies show they are positive for CD68, CD163, and lysozyme. The second are mesothelial cells, which have a cuboidal appearance, with less cytoplasm, and small nuclei, arranged in various patterns, including sheets, tubules, or even papillary structures. They show positivity for pan-keratins, CK 5/6, WT1, and calretinin. MICE collections lack supportive stroma, with both cell types embedded in fibrin.MICE pathogenesis remains a subject of debate. Two primary hypotheses have been proposed: one suggesting the lesion as a reactive phenomenon involving mechanical irritation, inflammation, or neoplasm triggering a reactive process and the other proposing it as an artifact resulting from surgical manipulation. While the artifactual hypothesis is deemed convincing for most cases, it falls short in explaining instances detected in patients without prior cardiac surgery.Despite their somewhat worrisome histological appearance, they show a benign clinical course, and additional treatment is rarely required. Therefore, the significance of recognizing this entity lies in its differential diagnosis, as an unaware pathologist may misinterpret it for a malignant neoplasm.While MICE as an entity has been recognized for several decades, benign histiocytic proliferations have been described in other sites of the human body. The similarities between some of them have been acknowledged, leading to attempts by some authors to consolidate all benign histiocytic proliferations into a single category. This group of benign histiocytic proliferations comprises:Reactive eosinophilic pleuritisHistioeosinophilic granuloma (HEG) of the thymusNodular mesothelial/histiocytic hyperplasia (NHMH)Mesothelial/monocytic incidental cardiac excrescences (MICE)- Celeste Santos Martins, MDReferencesMichal M, Kazakov DV, Dundr P, Peckova K, Agaimy A, Kutzner H, Havlicek F, Daum O, Dubova M, Michal M. Histiocytosis With Raisinoid Nuclei: A Unifying Concept for Lesions Reported Under Different Names as Nodular Mesothelial/Histiocytic Hyperplasia, Mesothelial/Monocytic Incidental Cardiac Excrescences, Intralymphatic Histiocytosis, and Others: A Report of 50 Cases. Am J Surg Pathol. 2016 Nov;40(11):1507-1516. doi: 10.1097/PAS.0000000000000687. PMID: 27340746.Censi S, Dell’Amore A, Conti R, Lorenzini P. Cardiac mesothelial/monocytic-incidental-excrescence: more than an artifactual lesion? Interact Cardiovasc Thorac Surg. 2008 Dec;7(6):1201-3. doi: 10.1510/icvts.2008.184499. Epub 2008 Sep 9. PMID: 18782786.Girolami I, Eccher A, Gilioli E, Novelli L, Di Stefano G, Brunelli M, Cima L. Mesothelial/monocytic incidental cardiac excrescences (MICE): report of a case and review of literature with focus on pathogenesis. Cardiovasc Pathol. 2018 Sep-Oct;36:25-29. doi: 10.1016/j.carpath.2018.06.001. Epub 2018 Jun 10. PMID: 30005394.Grossi VGR, Lee K, Demarchi LM, Castelli JB, Aiello VD. Occurrence of mesothelial/monocytic incidental cardiac excrescences in material from open-heart procedures: case reports and literature review. Autops Case Rep. 2018 Feb 27;8(1):e2018002. doi: 10.4322/acr.2018.002. PMID: 29515977; PMCID: PMC5828284.Veinot JP, Tazelaar HD, Edwards WD, Colby TV. Mesothelial/monocytic incidental cardiac excrescences: cardiac MICE. Mod Pathol. 1994 Jan;7(1):9-16. PMID: 8159657.
Case #74 / 23 – A coronary artery bypass graft site.
Coronary artery bypass grafting is a common procedure. Interpretation of these specimens at postmortem examination requires knowledge of the types of vessels involved.Firstly, there are two basic types of arteries: elastic and muscular. Elastic arteries are generally larger in caliber, and include the aorta, pulmonary artery, and the proximal branches of these arteries. During ventricular systole, these arteries need to absorb the volume and pressure of blood being ejected from through the semilunar valves. Abundant elastic fibers allow these arteries to distend to accommodate this volume change, then recoil in order to propel the blood forward and maintain diastolic blood pressure. The internal mammary arteries are the smallest caliber elastic arteries in the body.In contrast, muscular arteries are responsible for distribution of blood and thereby oxygen to peripheral organs. They have less elastic fibers and instead have condensed bundles of smooth muscle to aid in arterial constriction and relaxation. Examples of this type of artery include the coronary arteries and radial artery. Veins, on the other hand, have very little elastic fibers, and have a thin media composed of predominately smooth muscle.In returning to our case, the native coronary artery is on the right side of the image, which shows a muscular artery. The left side of the image shows an elastic artery. This elastic artery is the internal mammary artery, which is commonly used in bypass grafts.- Melanie Bois
Case #73 / 22 – A heart specimen was obtained from a feverish patient.
Acute rheumatic carditis (ARC) is a significant disease in certain parts of the world. It can result from rheumatic fever (ARF), which is a systemic poststreptococcal inflammatory disease. In general, ARF occurs 1-6 weeks after Group A (beta-hemolytic) Streptococcus pharyngitis. The M protein, expressed by Streptococcus, has structural overlap with cardiac myocyte proteins like myosin, tropomyosin and vimentin as well as endothelial cell components. This broad overlap leads to antibody cross-reactivity, and a pancarditis, wherein the myocardium, endocardium, valves, and pericardium can be affected.ARC manifests with a granulomatous reaction that can have fibrinous change to the center of the nodule. These nodular inflammatory foci are called Aschoff bodies/nodules (image below). Their appearance can look a little different depending on the phase of disease.The inflammatory cells characteristic of these lesions (though not specific) are the Anitschkow cells (see lower half of the image below). These cells are a modified macrophage with an elongated profile, slightly basophilic cytoplasm and a serrated chromatin bar. These have commonly been referred to as a “catepillar” cell, although they have an “owl eye” look when cut in cross-section. Fusion of Anitschkow cells into multinucleated giant cells result in Aschoff cells.- Melanie Bois
Case #72 / 21 – A temporal artery biosy was performed.e Choice Quiz
Figure A. Histologic evaluation for clinical suspicion of temporal arteritis is a common surgical specimen. However, a positive biopsy is only one of the 3 (of 5) criteria for the clinical diagnosis of temporal (giant cell) arteritis:Age >/=50 yearsNew headacheTemporal artery abnormality on physical examElevated inflammatory markers (ESR/CRP)Abnormal artery biopsyWhile a positive biopsy is highly specific, the sensitivity for this procedure is low (approximating 5-45%). This is due (in part) to the segmental involvement of the artery by giant cell arteritis (e.g. “skip lesions”). Positive cases have a unique microscopic appearance. It involved lymphohistiocytic inflammation involving the vascular media. However, notice that there’s no fibrinoid necrosis and no luminal thrombus. The vascular impairment and complications therein (such as blindness) result from intimal fibroplasia, unlike other types of vasculitides.Figure B. Alternate types of vasculitis may involve the temporal arteries. This is an example of polyarteritis nodosa. This disease is typified by the presence of fibrinoid necrosis, luminal thrombus, and mixed inflammationFigures C & D. In the case presented above, the clinical symptoms of giant cell arteritis were actually caused by amyloid deposition, rather than vasculitis. The literature shows that amyloid deposition in the temporal arteries is an uncommon mimic of giant cell arteritis. In general, the causative amyloid type is light chain (AL)-type amyloid. Such patients can have jaw- claudication, headaches, and even mildly elevated inflammatory markers. While an uncommon occurrence, it’s a good reminder to keep your differential broad, even on somewhat “routine” specimens. A polarized Congo red stain is included below.- Melanie Bois
Case #71 / 20 – A bioprosthetic valve is removed after 10 years.iz
Below is an image of a Ziehl-Neelsen stain for acid-fast bacilli, with numerous small acid-fast organisms consistent with Mycobacterium species. Mycobacterial infection of prosthetic valves are rare and can present years after the original surgical procedure. The vast majority are nontuberculous mycobacteria (NTM), such as M. chelonae, M. fortuitum, and M. abscessus. The diagnosis of this rare entity can be challenging, however, due to frequently negative blood cultures and sometimes minimal features of “classic” infectious vegetations, as would have been more likely for a Group A streptococcus infection.In this case, the organism was typed as Mycobacterium chimaera. M. chimaera infection has been associated with open heart surgery beginning in January 2012 through approximately the end of 2014. The infection was linked to heater-cooler devices used during surgery, and which were thought to be contaminated and aerosolizing the agent into the surgical field. Symptoms of infected individuals are insidious and non-specific, meaning that the microorganism can have time to disseminate and establish itself prior to detection. Most commonly, the histology is associated with granulomatous inflammation (as might be expected in a mycobacterial infection), with positive stains for acid-fast bacilli. Overall, the risk of infection in patients undergoing open heart surgery during this time period is extremely low, but nevertheless this entity should remain on the differential diagnosis in the right clinical circumstances.The CDC website contains additional information.- Melanie Bois
Case #70 / 19 – A 42-year-old man undergoes a heart biopsy.
Diffuse myocyte vacuolization necessitates a differential diagnosis of a storage disease, underlying mitochondrial disease, and cardiotoxicity. Electron microscopy is a useful tool in this differential.Storage disease (Fabry) vs cardiotoxicity (hydroxychloroquine). Two primary considerations for myocyte vacuolization are Fabry disease and hydroxychloroquine cardiotoxicity. They have a similar appearance on light microscopy with diffuse, irregular sarcolemmic vacuolization. Upon ultrastructural examination, both have concentric, laminated electron-dense structures called myeloid figures. However, hydroxychloroquine toxicity will have myelinoid figures and curvilinear bodies (right image), the latter of which are absent in Fabry Disease.Additional diseases can fall into the differential diagnosis, with unique ultrastructural findings. The SCVP has additional resources on interpretation of electron microscopy.- Melanie Bois
Case #69 / 18 – Name that valve!
The heart has two main types of valves: semilunar and atrioventricular. Semilunar valves include the aortic and pulmonary valves. These separate the ventricles from the great arteries, and open/close passively to preserve unidirectional blood flow. The cusps distend with backflow from the aorta and pulmonary artery, much like wind catches in a sail, resulting in valve closure. The photo in our question is an example of a semilunar valve. This is in contrast to atrioventricular valves, which include the mitral and tricuspid valves. They separate the atria from the ventricles and are composed of leaflets and a tensor apparatus (the tendinous cords and the papillary muscles).To distinguish between the pulmonary and aortic valve with just the image in the question, the anatomy of the outflow tract becomes important. While the valves themselves are similar, the pulmonary valve has an entirely muscular outflow tract (see arrows in this image). In contrast, the left ventricular outflow tract has a musculo (arrows)-membranous (asterisks) architecture just below the aortic valve, providing the important clue to this question’s answer.- Melanie Bois
Case #68 / 17 – A 35-year-old woman presents with rapid heart failure.
Although eosinophils are a dominant cell type in this image, the presence of the clear giant cell in the top left quadrant determines the diagnosis in this case of giant cell myocarditis.Giant cell myocarditis favors younger-to-middle aged adults and has loose associations with autoimmune disorders and thymoma/lymphoma (among others). Affected patients generally become symptomatically ill quickly. When this occurs, endomyocardial biopsy can be a helpful diagnostic tool to guide the clinical team (roughly half are diagnosed this way…with therapeutic implications). Histologically, one sees myocyte necrosis, giant cells, lymphocytes, and eosinophils, without truly well-formed granulomas. Interestingly, it may well be the eosinophils that cause the majority of the damage in this disease, not the giant cell for which it is named.In contrast, eosinophilic endomyocardial disease is uncommon and generally occurs in the setting of peripheral eosinophilia. As the eosinophils marginate in the ventricular chamber, they degranulate and cause localized (endocardial/subendocardial) damage to the myocardium. This results in relative blood stasis leading to thrombus formation and eventually endocardial fibrosis (generally with restrictive physiology). Patients tend to (but not always) present in the thrombosis stage, wherein they may show an intracardiac mass-like clinical presentation, or a thromboembolic one. On histology, thrombosis, endocardial fibrosis and eosinophilic myocarditis are present, but it is usually devoid of giant cells.More on myocarditis here.- Melanie Bois
Case #67 / 16 – A 49-year-old man undergoes heart transplantation.
The pattern of myocardial fibrosis in cardiac sarcoidosis is haphazard insomuch as it doesn’t occur in a single coronary artery distribution. Nor is the fibrosis limited to the subendocardium as one might encounter in atherosclerotic coronary artery disease. Rather, epicardial scarring is a prominent feature in this example (particularly in the anterolateral and lateral portions of the LV) while the subendocardium is spared. This pattern would be unlikely to occur in ischemia.While this pattern of fibrosis is seemingly random, propensities toward involvement of specific cardiac segments (e.g. the septum and inferoseptal myocardium) do become apparent in large series. As a reference, see this systematic review of sarcoid hearts.This disease is complex, and we are continuing to learn about its etiologies and presentations. However, it does seem to have an affinity toward the conduction system, wherein it can present clinically with arrythmias and (uncommonly) with sudden death.- Melanie Bois
Case #66 / 15 – A 38-year-old man died of unrelated causes.
The H&E photomicrograph shows cardiomyocytes with increased golden pigment, which is stained blue with an iron stain. This finding is pathognomonic for cardiac involvement from hemochromatosis, but it is interesting to note how subtle it can be on H&E alone.Hemochromatosis can be primary (from a germline mutation in – most commonly – the HFE gene), or secondary from chronic iron or RBC transfusions (e.g. thalassemia). The disease is associated with a host of systemic symptoms, including endocrinopathies, skin pigmentation, weakness, fatigue, and arthritis.In the heart, excess iron is toxic. Circulating free iron enters the cardiomyocytes via calcium channels and is catalyzed by the rapid Fenton reaction to produce free radicals. These, in turn, damage the cell membranes resulting in cell dysfunction and ultimately, cell death.While very early stages of disease have been associated with restrictive physiology, the cardiomyopathy (or, more accurately, the cardiotoxicity) resulting from excess iron deposition is actually of the dilated variety.- Melanie Bois
Case #65 / 14 – A 1-year-old girl has a mass resected.
The photomicrograph shows the classic vacuolated cells of a cardiac rhabdomyoma, the most common cardiac neoplasm in infants and children. Roughly 4 out of every 5 cardiac rhabdomyomas are associated with tuberous sclerosis. Under the microscope, these tumors are heavily glycogenated with radial spokes of sarcoplasm emanating from central contractile elements, giving the moniker of a “spider cell”.Interestingly, a subset of cardiac rhabdomyomas will undergo spontaneous regression. As such, surgical resection is somewhat uncommon and reserved for symptomatic cases. mTOR inhibitors have also be used to hasten their regression.The differential diagnosis based on the question distractors are as follows:Neurofibromas in the setting of neurofibromatosis can develop in the heart, but this is rare by comparison.Nevoid basal cell carcinoma (Gorlin) syndrome is associated with cardiac fibromas, the second most common cardiac neoplasm in children.Carney complex is associated with cardiac myxomas, which manifest predominately in an adult population- Melanie Bois
Case #64 / 13 – A 47-year-old man has a valve resected.
The gross pathology shows lobulated, friable red-tan heterogeneous vegetations involving all cusps. The cusp on the right side of the image shows damage inferiorly by the vegetation. This combination of vegetations with concomitant tissue damage is virtually pathognomonic for infective endocarditis.What is the most common organism causing infective native valve endocarditis? This reference studied 310 valves, with 44 different organisms (https://www.sciencedirect.com/science/article/pii/S1054880712000610).“The four most commonly identified organisms were viridans group streptococci (28%), Staphylococcus aureus (18%), enterococci (9%), and coagulase-negative staphylococci (8%).” All of these are Gram-positive cocci.With regard to the differential diagnosis, non-bacterial thrombotic endocarditis (NBTE; choice C) is sterile and composed of platelets and fibrin. It’s associated with underlying hypercoagulable conditions such as autoimmune disorders and malignancy. The mitral valve is most commonly affected, followed by the aortic valve in frequency. NBTE classically occurs along the lines of closure of the valve. The endocardial irritation that occurs in that location may serve as a nidus for development. They tend to have a smoother contour, are usually more uniformly red in coloration, and do not cause underlying valve damage. They have a “stuck on” appearance, rather than an erosive one.Papillary fibroelastoma/ Lambl excrescence (PFE / LE) was also in the differential (choice D). The projection emanating from the bottom cusp is suspicious for this. However, PFE/LE does not cause underlying valve damage, and (2) the associated vegetations are not in keeping with this diagnosis. Here’s a gross photo for reference.- Melanie Bois
Case #63 / 12 – A 62-year-old man still has cardiomyopathy.
Recall that in our last case, we discussed the composition and folding of amyloid as a misfolded protein depositing in beta-pleated sheets. Amyloid is interesting, because the primary protein isn’t necessarily constant. In fact, there are over 30 different proteins that can deposit as amyloid, designated with an “A” and then their protein abbreviation. Twelve have been described in the heart (see figure below; https://www.sciencedirect.com/science/article/pii/S105488071500085X).Of those, the dictum is that 80% of amyloid in the heart is AL. A little less than 20% is ATTR, and the tiny fraction that’s left over is distributed among the very uncommon other types. The type of amyloid influences treatment. Treating light chain amyloidosis (AL) involves chemotherapy to address the underlying plasma cell dyscrasia. ATTR has new treatments that stabilize the transthyretin molecule to prevent it from aggregating abnormally.After establishing a diagnosis of amyloidosis, the next step is to determine which kind it is due to the aforementioned treatment implications. Can you use light microscopy to do so? There are trends that are highly suggestive of one type over another (https://pubmed.ncbi.nlm.nih.gov/26212778/).These authors categorized deposition as pericellular (lacelike, image A) or nodular (cannon ball, image C below).AL more commonly deposits in a pericellular distribution, and ATTR is more commonly nodular (see data below). However, there’s enough overlap that you can’t allocate patient treatment based on these patterns. You must confirm the amyloid type for accurate prognostication and therapy. There’s a number of methodologies employed to accomplish this.- Melanie Bois
Case #62 / 11 – A 62-year-old man with cardiomyopathy.
The hematoxylin and eosin image (taken at 200x original magnification) shows somewhat shrunken-appearing cardiomyocytes surrounded by lace-like, eosinophilic extracellular material. The differential, based on the H&E image, includes interstitial fibrosis and amyloidosis. This differential can be quite challenging, especially when there’s little material to evaluate.The classic stain used to confirm amyloid deposition is Congo red, which intercalates into the beta-pleated sheets of amyloid proteins and is held there via hydrogen bonds. Congophilic material that also demonstrates birefringence under cross-polarized light is considered specific for a diagnosis of amyloid (see image).The downside is that Congo red is a technically challenging stain to perform and read. Overstaining can result in non-specific deposition; under-staining can cause a lack of sensitivity. Moreover, collagen will polarize (adding to the confusion), but its polarization is more of a whitish color rather than the birefringence of amyloid.Sulfated Alcian blue is the special stain pictured in the question. Alcian blue stains mucopolysaccrides, not amyloid itself. Nevertheless, in organ systems with minimal naturally occurring glycoaminoglycans, it can be a very useful tool to highlight amyloid.Amyloid is composed of a misfolded extracellular fibrillary protein, but it also contains other material including a non-fibrillary glycoprotein: (serum) amyloid P (SAP) component. SAP binds to glycoaminoglycans and other cellular components, incorporating those into the amyloid matrix. Thus, sulfated Alcian blue stains the mucopolysaccrides that are associated with amyloid deposits, but not amyloid itself.For this reason, sulfated Alcian blue is a sensitive stain in the heart for amyloid (generally allowing for easy detection in tissue), but not specific. Confirmation via a Congo red stain is recommended, with its telltale birefringence.- Melanie Bois
Case #61 / 10 – A 46-year-old with inflammation.
The histopathology shows myocytes involved by a lymphocytic inflammatory process causing multifocal myocyte damage. The appearance is diagnostic of an active lymphocytic myocarditis.The diagnosis of active myocarditis based on the Dallas criteria, which requires inflammation of the myocardium with myocyte injury/damage that is not characteristic of ischemic injury.Commonly accepted criteria for myocyte injury include lymphocytic “scalloping” of the sarcolemmic border (see arrows in photo), loss of cross-striations, and hypereosinophilia of the myocyte. If you have inflammation in the absence of myocyte damage, the proper diagnostic terminology is “borderline [inflammation type, e.g. lymphocytic] myocarditis”.With regard to the differential diagnosis, borderline [lymphocytic] myocarditis shows the relevant inflammation, but without myocyte damage. The distinction can be exceptionally challenging at times.Sarcoidosis is typified by tight, non-necrotizing granulomatous inflammation. The image shows a predominance of lymphocytic inflammation, without granuloma. It’s been loosely associated with Propionibacterium.Giant cell myocarditis (GCM) has both giant cells (as the name implies) as well as eosinophils. The cause of GCM is unknown. Roughly 1/5 of individuals have an underlying autoimmune disease, making this a compelling association.Myocardial infarctions may look different depending on the age of the lesion, but most commonly show neutrophilic inflammation, followed by macrophages, and fibroblasts. Lymphocytes aren’t a predominate part of the picture in this disease process.- Melanie Bois
Case #60 / 9 – A pericardial finding.
This is the “bread and butter” look of pericarditis.Pericarditis has numerous potential causes: acute MI, surgery, infection, uremia, connective tissue diseases, and neoplasia. Uremia can be caused by underlying renal injuries. Thus, at the time of autopsy, it’s important to consider chronic or acute renal disease in the differential of a patient who died with this findingThis Letter to the Editor lists one institution’s experience with pericarditis at the time of autopsy, detailing a 10% prevalence of uremia among 30 decedents with pericarditis.- Melanie Bois
Case #59 / 8 – An unusual cardiac infection.
Chagas disease is a public health issue in Central and South America, where the triatomine bug (a type of reduviid bug) is common.This insect is sometimes known as the kissing bug, or vampire bug, because it’s drawn to the carbon dioxide exhaled from the mouth and nose and feeds in this location during the night (when the bug is most active). It can carry the parasite Trypanosoma cruzi, which is transmitted via the bug’s feces while it’s feeding near a person’s mucous membranes. Accidental rubbing of those feces into the mouth or eyes can cause transmission. The classic sign associated with this disease is unilateral eyelid swelling resulting from acute infection, so-called Romaña’s sign. Note that other forms of transmission are possible.Once infected, cardiac involvement takes the form of an acute phase (which is rare), followed by an intermediate/chronic phase (more common). The acute phase, which was shown in the question photos, can be mild or asymptomatic, but may also manifest with a serious (sometimes fatal) myocarditis. The chronic form is more insidious, and likely affects millions of individuals in the endemic areas. This disease manifests as a dilated cardiomyopathy, with variable apical left ventricular aneurysm formation, along with interstitial lymphoplasmacytic inflammation. The conduction system abnormalities can be significant and variable in presentation. This image, by the American Heart Association summarizes the manifestations of Chagas Cardiomyopathy. For more information, this article is recommended.Photo credits: CDC, courtesy of James Gathany; accessed: www.cdc.gov/parasites/chagas/gen_info/vectors/index.html; credit: WHO/TDR, access: www.cdc.gov/parasites/chagas/gen_info/detailed.html; www.ahajournals.org/doi/full/10.1161/CIR.0000000000000599.- Melanie Bois
Case #58 / 7 – A mass in a 66-year-old woman.
Cardiac myxomas can be heterogeneous under the microscope. They are said to arise from pluripotent mesenchymal stem cells, which means that they can undergo somatic differentiation. Their diagnostic cell, the lepidic (myxoma) cell, has basophilic cytoplasm with long processes, and bland ovoid nuclei. Classically, they form vasotropic rings around the small vessels within the tumor.Because these tumors can be present for months to years prior to resection, they can undergo calcification. Also, depending on their location, they can be prone to hemorrhage from turbulent blood flow and contact with nearby endocardium. As the hemorrhage breaks down, it can deposit on fibrous and elastic tissue (along with calcium) to form so-called Gamna-Gandy bodies. These are most commonly seen in the spleen (same pathophysiology) but may also be seen in myxomas.- Melanie Bois
Case #57 / 6 – A 78-year-old woman died of aspiration pneumonia.
The x-ray shows a C-shaped radiopaque mass encircling the annulus of the mitral valve (left side of the image). In the additional image is a base-of-heart dissection of a different case, showing the valves in the same layout for correlation to the x-ray. This radiopaque material is known as mitral annular calcification or MAC. It is a degenerative phenomenon in which calcific deposits occur along the mitral valve annulus in response to increased afterload (e.g. aortic stenosis, systemic hypertension, or hypertrophic cardiomyopathy). Women are more likely to develop MAC than men.In general, MAC a benign phenomenon, and not uncommon to encounter (in a mild form) at autopsy. When it becomes significant and mass-like, however, it can interfere with leaflet coaptation leading to mitral regurgitation, or to stenosis by obstructing the mitral valve opening. Rarely, the calcification can erode or impinge on the atrioventricular node, causing arrhythmias and/or sudden death. Other complications include thromboemboli, and endocarditis.- Melanie Bois
Case #56 / 5 – A 49-year-old underwent cardiac surgery.
Congenitally bicuspid aortic valves (BAV) occur in 1-2% of the population. Of those individuals, roughly half will have an ascending aortic aneurysm (AscAA). AscAA puts patients at risk for dissection and rupture, a potentially fatal complication due to bleeding into the pericardium. About a third of patients with BAV have first degree family members with an enlarged ascending aortas as well, even if their aortic valve is normal. This has important implications for screening in the clinical realm.The specimen in the question is a congenitally bicuspid aortic valve (BAV). First and foremost, there are two cusps. Several features can assist in the proper identification of a congenitally bicuspid aortic valve versus a tricuspid aortic valve with two (apparent) cusps due to acquired commissural fusion. Misdiagnosis can lead to unnecessary testing of (and health care spending dedicated to) the patient and his/her family members. Congenitally BAV have (1) uneven cusp size between the two cusps, (2) raphe (juncture of the two conjoined underdeveloped cusps), (3) obtuse angle of the conjoined (larger) cusp. The fenestrations are degenerative changes that can occur in tricuspid and bicuspid aortic valves.BAVs do not have an association with cardiac amyloid, pericarditis, or pulmonary hypertension. Mitral stenosis could be associated with a postinflammatory aortic valve specimen; however those aortic valves have commissural fusion, cusp thickening, and a “candle-wax” appearance.- Melanie Bois
Case #55 / 4 – An atherosclerotic plaque.
Plaques are dynamic often driven by the processes of inflammatory cells. The more potential for movement, the more likely they are to rupture. Rupture will (usually) result in downstream embolization and/or thrombosis.Calcification, adventitial fibrosis, and circumferentail plaque distribution are all factors that harden the plaque, stabilize it, or are more protective of the plaque. Calcification, when it occurs in atherosclerotic plaques, tends to create a more stable plaque. Adventitial fibrosis would also stabilize the plaque as well by reinforcing the arterial wall. Interestingly, a circumferential distribution of atherosclerotic disease will also stabilize the lesion when compared to an eccentric location within the arterial intima.Inflammation will destabilize a plaque. Similarly, the other factors listed in the attached image (eccentric distribution, necrotic core, thin fibrous cap, angiogenesis) contribute to the instability of a plaque.- Melanie Bois
Case #54 / 3 – An 87-year-old woman was found deceased.
Hemopericardium is present in the question image, as evidenced by the discoloration and bulging of the pericardial sac. Hemopericardium can occur for numerous reasons, the most common of which are ruptured myocardial infarction (MI) and rupture of an ascending aortic aneurysm/dissection. Risk factors for myocardial rupture after MI include: older, female, systemic hypertension, first MI. Risk factors for ascending aortic aneurysm and dissection include bicuspid aortic valve, connective tissue disease, inflammatory aortopathy, smoking, systemic hypertension, and prior family history.The commonality for both is uncontrolled systemic hypertension. In this case, this patient had an ascending aortic aneurysm rupture (see left photo, white probe), with a dissection tract (see right photo, white arrow), however she could have had a ruptured MI due to underlying hypertension as well, with the same outcome.Admittedly, a case could be made for the answers of end-stage renal disease and myxomatous mitral valve; although they are not “most likely” to have resulted in the patient’s condition. End-stage renal disease is frequently associated with atherosclerotic disease and long-standing systemic hypertension. However, with one of the answer choices being “systemic hypertension”, this is a more direct response.Myxomatous mitral valve disease can be associated with an underlying connective tissue disease. Such syndromes (e.g. Marfan) have marked concomitant aortopathies, which can lead to rupture and hemopericardium. However, these generally occur earlier in life than the patient presented in our case.- Melanie Bois
Case #53 / 2 – A 78-year-old woman with coronary artery disease.
This is a hydrophilic polymer embolus with surrounding giant cell reaction. Hydrophilic polymers are ubiquitous on intravascular devices, used to decrease friction and the chance of damage to the vessel wall. However, separation of this material from the medical device has been documented to result in polymer embolization in a variety of organs. Histologically, it’s generally described as an amorphous or serpiginous basophilic substance with concurrent foreign body reaction. Here’s a comprehensive review on the topic.With regard to the differential diagnosis, heart worm (Dirofilaria) is primarily a zoonotic parasite; however, humans can also be infected (but are suboptimal hosts) . When humans acquire the disease from a mosquito bite, the dying worms generally end up in the small pulmonary arteries, producing multifocal granulomas. Most cases are thought to be subclinical, though a minority may present with hemoptysis, fever, or a pleural effusion. It’s primarily an intravascular disease… so its presence in the myocardium (like in the question’s photo) would be unlikely. This article provides additional details.Loa loa is another parasite that is transmitted by the deerfly. Disturbingly, this parasite can create visual movement across the surface of the eye, and sometimes under the skin. It has rarely been associated with heart disease but could potentially cause peripheral eosinophilia that could results in endomyocardial fibrosis.Amyloid is an extracellular, amorphous eosinophilic material; in contrast to this basophilic, serpiginous substance.Basophilic degeneration is a compelling choice because of the color of this substance. However, this is an age-related phenomenon resulting in globular basophilic deposits within cardiomyocytes (not giant cells), that are strongly PAS-positive (see image).- Melanie Bois
Case #52 / 1 – A 48-year-old man underwent tricuspid valve replacement.
Gross findings: Carcinoid heart disease presents as white-tan “stuck-on” plaques on valves and endocardial surfaces. Classically, it will lack disruption of the underlying valve itself, distinguishing it from destructive lesions like endocarditis, and acquired structural changes like myxomatous disease and postinflammatory (rheumatic) disease. The plaques hinder a valve’s ability to move and thus results in functional disruption (regurg, stenosis, or mixed disease). Note also that there is no tumor in carcinoid heart disease. It also preferentially affects the right heart.What gross features and clues in the history helped with the differential?Ebstein is a failure of the tricuspid valve to develop properly. The valve peels up from the RV wall during formation, and this disease generally results from a premature failure of that process. Thus, the TV is usually apically displaced, sometimes incomplete, and generally quite thin. Moreover, surgical resection of TV in Ebstein is uncommon.Rheumatic valves have a thickened “dipped in candle wax” appearance, with fusion and foreshortening of the cords. This answer is certainly in the differential on a strictly gross finding basis, though it most commonly affects all valves equally, or favors the left sided valves.Degenerative fibrocalcific changes are extremely uncommon in the tricuspid valve. This change mostly affects those valves exposed to higher pressures (left-side), and with aortic valve comprising the majority of this diagnosis.Endocarditis could manifest with right-sided predilection, particularly in an intravenous drug user. It could also present with mass-like valvular lesions, but nearly universally shows underlying valve destruction. However, in this case, the cords look abnormal too, not just the valve. Normal cords should be thin and pliable, not thickened, fused, shortened and white like seen here.More about this amazing disease:The interaction of serotonin and other vasoactive compounds elaborated by a carcinoid tumor with the endocardium can result in this pathology.Serotonin is metabolized to 5-hydroxyindoleacetic acid (5-HIAA) by monoamine oxidase and aldehyde dehydrogenase. This occurs in the liver, lungs, and (to an extent) brain. If serotonin bypasses hepatic metabolism and drains directly into the inferior vena cava (either from hepatic mets or a gonadal primary), it exposes the right heart to the serotonin-rich blood. The current theory hypothesizes that the presence of monoamine oxidase in the lungs leads to serotonin metabolism before the blood reaches the left heart, thereby sparing the mitral and aortic valves and leading to an exquisitely right-sided presentation (hence the tricuspid valve pathology in this case). Rarely, lymph node metastases may also contribute to carcinoid heart disease via thoracic duct drainage.Serotonin receptors on the cardiac valves are activated by the serotonin-rich environment, leading to the classic histologic picture of fibroproliferative spindle cells with tapered ends in a loose, myxoid background. These lesions have a “stuck on” appearance on microscopy, affecting the upstream surface of the valve without damage to the underlying valvular architecture (as pictured in the VVG attachment).The most common valvulopathies associated with carcinoid heart disease are tricuspid valve regurgitation and mixed pulmonary valve insufficiency and stenosis. This occurs due to valvular retraction, fibrotic thickening, and commissural fusion. As seen in the gross image, the chordae tendineae are foreshortened, thickened, and fused in this disease.The presence of carcinoid heart disease is associated with a worse three-year survival in patients with carcinoid syndrome, emphasizing the importance of recognizing this disease on surgical pathology. For more information see this review by Hassan et al.
A 50-year-old man undergoes a heart transplant for a familial cardiomyopathy.
Click here for the answer.
Lamin A/C Cardiomyopathy
Click here for a discussion of the entity.
Lamin (LMNA) A/C mutations typically cause a dilated cardiomyopathy appearance. While this heart grossly had that appearance, it also had significant fibrofatty replacement of the right ventricle free wall, particularly along the outflow track. This gives the appearance of arrhythmogenic right ventricular cardiomyopathy (ARVC), one of the arrhythmogenic cardiomyopathy diseases. This overlap has been described and some ARVC cases are reported as having LMNA mutations.
Fetal loss in the 22nd week of gestation due to severe arrhythmia (third-degree AV block). The mother suffers from Sjögren syndrome and autoimmune thyroiditis. She delivered another baby previously, affected by neonatal lupus.SCVP thanks Ondrej Fabian for sharing this case.
Click here for the answer.
Calcified and fibrotic conduction system (AV node and part of the bundle branch).
Click here for a discussion of the entity.
Congenital heart block can be associated with various prenatal conditions including structural heart malformations, neonatal lupus or various intrauterine infections. The outcome depends largely on the presence of the underlying structural disease. If the heart block is diagnosed during the fetal period, there is a very high rate of fetal and neonatal loss. If the block is first diagnosed in the newborn period, the prognosis is better. A histopatological examination may reveal an extensive fibrosis, multinucleated giant cells, inflammation, calcifications or poorly developed AV node or other parts of the conduction system.
A 3 year old boy developed a 7 cm tumor of the left ventricle. It was excised.SCVP thanks Ondrej Fabian for sharing this case.
Click here for the answer.
Cardiac fibroma.
Click here for a discussion of the entity.
Cardiac fibroma is generally rare, but represents the second most common cardiac neoplasm in childhood. The tumor doesn’t embody an aggressive behaviour. However, its infiltrative pattern and frequent large diameters often result in positive surgical margins. The main differential diagnosis is a fibrosarcoma, as the fibroma itself can be quite cellular. However, fibrosarcomas are exceedingly rare in children.
A 56-year-old woman with had a history of a “submandibular tumor.” Recently, a pericardial mass was found and extirpated.SCVP thanks Ondrej Fabian for sharing this case.
Click here for a discussion of the entity.
A metastatic neoplasm from other primary locality is the most common type of heart tumor. The most frequent are melanoma, lymphoma or carcinoma of the lung, breast and oesophagus. Cardiac involvement by metastatic salivary malignancy is extremely rare, described in single case reports only.
Click here for the answer.
Metastatic adenoid-cystic carcinoma.
A 1 and a half year old girl had failure to thrive. Additionally, she had muscular hypotony, chronic dyspnea, and lactate acidosis. Signs of systolic heart failure appeared over two months. Echocardiography demonstrated a dilated cardiomyopathy and an endomyocardial biopsy was performed. The girl ultmiately underwent a heart transplant and images from the transplant are seen.SCVP thanks Ondrej Fabian for sharing this case.
Click here for the answer.
Mitochondrial cardiomyopathy.
Click here for a discussion of the entity.
A histopathological examination of the endomyocardial biopsy plays an important role in the diagnosis of metabolic cardiomyopathies and can direct clinicians towards the enzymatic analysis and genetic testing. In case of primary mitochondrial disease, the clinical setting (muscular hypotony, lactate acidosis, stroke-like episodes,…) if often suggestive. At the gross examination, hypertrophic pattern of cardiomyopathy is the most typical. Microscopically, there is a vacuolization of the cardiomyocytes with numerous mitochondria including giant forms (seen within the green circle). By ultrastructure, numerous mitochondria of abnormal shape and size are found.
A 37 year-old-woman developed a ruptured intracranial aneurysm. During the neurosurgical procedure, a sudden heart failure developed, with dilatation of the ventricles, especially in the apical portion. The woman died shortly afterwards and served as a multiorgan donor. Images of her heart are seen.SCVP thanks Ondrej Fabian for sharing this case.
Click here for a discussion of the entity.
A catecholamine induced cardiomyopathy is a stress-related disease. The diagnosis is largely based on clinical criteria. On the gross examination, there is a dilatation of the ventricles often affecting the apical portion of the heart. Microscopically, prominent contraction bands, with or without myocyte necrosis, are typical features, together with sparse mixed inflammatory infiltration, oedema and haemorrhages.
Click here for the answer.
Tako-tsubo cardiomyopathy.
A 67-year-old woman developed recurrent pericardial effusions. Repeated cytology of the effusion showed inflammatory cells and was negative for malignancy. Systolic heart failure increased and the subject underwent pericardial fenestration. Biopsy materials of the epicardium was collected at that time.SCVP thanks Ondrej Fabian for sharing this case.
Click here for a discussion of the entity.
A lobular carcinoma of the breast represents one of the most common secondary heart tumors. Pericardial involvement with recurrent effusions is one of the typical clinical presentations. However, no physical or laboratory examination can specifically detect cardiac metastases in case of diffuse disease. Therefore, it can be easily misdiagnosed as a myocarditis or another non-neoplastic condition.
Click here for the answer.
Metastatic lobular breast carcinoma.
A 59-year-old woman with no significant past medical history had a one day history of malaise, chest discomfort, and nausea and vomiting. She had a cardiac arrest and resuscitation attempted. She did not survive and an autopsy was performedSCVP thanks Michael Seidman for sharing this case.
Click here for a discussion of the entity.
Acute myocardial infarctions with septal wall rupture have become less frequent, but still a cause of sudden death. While maximal likelihood of rupture is thought to be ~5 days post myocardial infarction, ruptures can occur throughout the first week or so. The history of this case suggests rupture occured on day 2. Sarcoidosis can appear almost anywhere in the body. Cardiac sarcoidosis is the third most common location of sarcoidosis and carries the most significant morbidity and mortality risk.
Click here for the answer.
Ruptured acute myocardial infarction secondary to atherosclerotic plaque rupture. Also, incidental non-cardiac sarcoidosis.
A 63-year-old man has a history of giant cell myocarditis. He had this entity noted on the explantation of his first heart transplant, which was being replaced for transplant arteriopathy.SCVP thanks Greg Fishbein for sharing this case.
Click here for the answer.
Catheter sheath embolus.
Click here for a discussion of the entity.
This finding can be confused with an organism. However, it is hydrophilic polymer material from a presumed earlier left heart catheterization. This entity was further described here: Mehta RI et al. Hydrophilic polymer emboli: an under-recognized iatrogenic cause of ischemia and infarct. Mod Pathol; 2010;23:921–30
A 47-year-old woman presents to the hospital with a 3 month history of shortness of breath. Prior echocardiogram was unremarkable. Cardiac MRI one month prior showed late gadolinium enhancement and a troponin was 0.3. A Cardiac PET/CT at last admission showed patchy diffuse hypermetabolism. A biopsy was performed.
Click here for the answer.
Probable Sarcoidosis.
Click here for a discussion of the entity.
This is an unusual case in that it has features of both giant cell myocarditis and sarcoidosis. The infiltrative pattern, with adjacent myocyte injury along with numerous eosinophils favors giant cell myocarditis. The large “fluffy” giant cells with inclusions reminiscent of asteroid bodies, are more typical of sarcoidosis. It may be there is an intermediate group of less aggressive giant cell myocarditis cases or more agressive sarcoid cases that have this histopathology. Indeed, this case was not hyperagressive as typical of other giant cell myocarditis cases. Drs. Maleszewski and Halushka are interested in studying this intermediate entitity. If you have a case and would be interested in sharing it, for such a study, please contact Marc Halushka.
A 67-year-old woman who had a heart transplant 3 years earlier presented for a routine heart biopsy in normal health.
Click here for the answer.
Antibody mediated rejection, pAMR1 (H+).
Click here for a discussion of the entity.
In 2013, the ISHLT instituted a new nomenclature for pathologist-directed diagnosis of AMR, termed pAMR. This case has the classic histomorphometric appearance of AMR as described in our AMR tutorial. Namely there is a “busy B” pattern at low power and at high power significant numbers of intravascular mononuclear cells are seen. Interestingly for this patient, complement staining for C3d and C4d was negative. A DSA was not elevated, although there was increased cross-reactivity to more HLAs. Thus, the best diagnosis for the patient is pAMR1 (H+). This is not always treated the same as AMR that causes positive C4d and C3d staining.
A 75-year-old woman presented to the hospital with heart failure that progressed for some time but worsened in the past two weeks, and a remote history of seizure disorder and lupus. An endomyocardial biopsy was performed.
Click here for a discussion of the entity.
Whenever there is a suspicion of lupus myocarditis, and a patient is taking Plaquenil, it is a good idea to perform EM. On the light microscopy, there was no evidence of inflammation, but there was evidence of myocyte vacuolization and granular material. This material was slightly larger than lipofuscin.
Click here for the answer.
Hydroxychloroquine (Plaquenil) Cardiomyopathy.
A 36-year-old man died suddenly. At age 9 he had a pacemaker implanted, but at age 20 it was removed and not replaced. Autopsy showed the following lesion in the AV node.Thank you to Dr. Greg Fishbein for sharing this case.
Click here for a discussion of the entity.
Cystic tumor of the AV node is a benign heterotopia of endodermal origin. They can cause heart block and, as seen in this case, are a cause of sudden cardiac death. They have been described as the smallest tumor that can kill The tumor is comprised of cysts lined by cuboidal cells in a two-cell population. More information can be found in the AFIP Atlas of Tumor Pathology Series 4 – Tumors of the Heart and Great Vessels.
Click here for the answer.
Cystic tumor of the AV node.
A 46-year-old woman presents for a routine endomyocardial biopsy after transplantation roughly 2 years after her transplant. By report the patient was feeling well. Four pieces of tissue were obtained.
Click here for a discussion of the entity.
Quilty lesions are benign collections of lymphocytes. They are known mimickers of rejection. By the H&E, the wide discrepancy in the amount of inflammation on the one piece versus the other pieces suggested it was not likely to be rejection. A CD21 is not very sensitive, but it is specific for a Quilty lesion. Reference: The presence of a CD21+ follicular dendritic cell network distinguishes invasive Quilty lesions from cardiac acute cellular rejection. There is a small focus of rejection on one piece of tissue earning the designation of 1R.
Click here for the answer.
Quilty lesion and 1R rejection.
A 26-year-old woman is diagnosed with hypertrophic cardiomyopathy and asymmetric septal hypertrophy. Endomyocardial biopsy was performed.Thank you to Dr. Greg Fishbein for sharing this case.
Click here for a discussion of the entity.
Histopathologically there are markedly vacuolated cardiomyocytes. These cells contain PAS positive granules and a PAS- diastase (PAS-D) will be negative. This entity is a mimicker of hypertrophic cardiomyopathy.
Click here for the answer.
Glycogen storage cardiomyopathy caused by a PRKAG2 mutation.
A 73-year-old woman is diagnosed with a 6 cm right ventricle mass that is adherent to the tricuspid valve. Surgery was performed to remove it.
Click here for a discussion of the entity.
Synovial sarcomas represent 3-5% of primary heart sarcomas. They can be of three different types: biphasic, monophasic and poorly differentiated, of which the monophasic type is the most common in the heart. These cases are positive for vimentin and EMA in most cases and less frequently positive for pan-cytokeratins, synaptophysin and CD99. This particular case was strongly BCL2 positive. Information from: AFIP Atlas of Tumor Pathology.
Click here for the answer.
Synovial Sarcoma, Grade 2, Monophasic Fibrous Type.
A 20-year-old male presents with a myocardial infarction. Cardiac catheterization reveals dilated coronary arteries with thrombus material in one. Surgery was performed to remove the proximal coronary vessels.
Click here for a discussion of the entity.
Early in the Kawasaki disease pathogenesis there can be an acute necrotizing arteritis. That leads to injury and loss of the internal elastic lamina. This case is late in the process after the injury occurred and the inflammation is predominately in the adventitia.
Click here for the answer.
Healed and late Kawasaki’s disease of the coronary.
An 66-year-old female died of a retroperitoneal hematoma secondary to anticoagulation and an autopsy was performed.
Click here for a discussion of the entity.
Advanced thymic carcinoma routinely invades the heart due to the close proximity of the thymus to the heart.
Click here for the answer.
Thymic carcinoma infiltrating the heart.
An otherwise healthy 45-year-old male underwent left ventricular assist device placement four days after a large myocardial infarction.
Click here for a discussion of the entity.
The presence of large atypical cells with frequent mitoses within vascular spaces was highly unexpected. The differential diagnosis included intravascular lymphoma. However, the positive E-cadherin and myeloperoxidase with negative B and T cell markers demonstrated that this was extramedullary hematopoiesis (EMH). EMH can occur throughtout the body and has been demonstrated previously in the heart. REFERENCE: Hill and Swanson “Myocardial extramedullary hematopoiesis: a clinicopathologic study .” Mod Pathol 2000.
Click here for the answer.
Extramedullary hematopoiesis in a background of a large myocardial infarction.
A 79-year-old woman underwent autopsy for an intraperitoneal hemorrhage. This mass was found in her heart.Thank you to Dr. Austin McCuiston for sharing this case.
Click here for a discussion of the entity.
This is an exuberant and tumor-like lesion that is an expansion of the more common mitral annular calcification. It can be extruded out of its capsule and become expansile. There can be external granulation tissue surrounding calcifications with a central softened (pasty) interior (images 6 and 7).
Click here for the answer.
Mitral annular calcification resulting in pseudotumor (Caseous Calcification)
A 65-year-old male underwent routine biopsy for cardiac transplantation surveillance.
Click here for a discussion of the entity.
Rare patients have these extensive and deep Quilty lesions that can be deep in the tissue away from the epicardial surface. Quilty lesions have increased numbers of CD20+ cells as seen in this example. This case also nicely demonstrates positive CD21 staining which is specific for Quilty lesions. The presence of CD21 in the deep lesions indicates these were Quilty lesions and not higher level rejection. The patient was not treated and continues to do well.
Click here for the answer.
Extensive and deep Quilty lesions and mild (1R) rejection.
A 43-year-old alcoholic male was found dead in bed. Toxicology demonstrated an alcohol level of 198 mg/dl. An autopsy was performed.Thank you to Dr. Mary Sheppard for sharing this case.
Click here for a discussion of the entity.
This case also featured a congenital bicuspid aortic valve and an anomalous coronary artery origin. The vegetation seen in the first image could easily be mistaken for a large lambl’s excrescence or a small fibroelastoma.
Click here for the answer.
Endocarditis and infectious thrombi.
A 62-year-old male developed aortic valve stenosis. Surgery was performed.Thank you to Dr. Joseph Maleszewski for sharing this case.
Click here for a discussion of the entity.
Ochronosis of the aortic valve is a manifestation of chronic alkaptonuira that is the caused by deposition of bluish-black pigment consisting of oxidized homogentisic acid. The metabolic derangement is the result of a recessive trait. Pigment can deposited in intervertebral discs, cartilage, skin and cardiac valves (particularly the aortic and mitral valves). Heavy calcification is often seen in association with the pigment (as in this case) and there is a general belief that the pigment hastens development of both atherosclerosis and calcification. This may, in part, explain the relatively young age (60-years-old) that this patient developed hemodynamically significant (tricuspid) aortic valve stenosis, which is usually seen in the 8th or 9th decades of life.
Click here for the answer.
Ochronosis.
A 62-year-old female was being worked up for pneumonia when she was discovered to have a 2.6 cm right ventricular mass. Surgery was performed.Thank you to Dr. Pedram Argani for sharing this case.
Click here for the answer.
Hemangioma
A 67-year-old female with a past history of breast cancer developed a B-cell lymphoma. THe patient developed complications during a donor bone marrow transplant and died. An autopsy was performed.Thank you to Dr. Marissa White for sharing this case.
Click here for the answer.
Toxoplasmosis
A 47-year old female was diagnosed with heart failure ascribed clinically to idiopathic DCM, ultimately requiring transplant. The explanted heart is shown. What was the real cause of her heart failure?Thank you to Dr. Michael Seidman for sharing this case.
Click here for the answer.
Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC).
A 32 year-old male had progressive muscle weakness since age 10 and was wheelchair bound by age 18. He had progressive congestive heart failure with eventual development of lethal pulmonary emboli. At autopsy, the heart appeared as follows. What was his diagnosis?Thank you to Dr. Michael Seidman for sharing this case.
Click here for the answer.
Becker muscular dystrophy-associated DCM (dystrophinopathy, etc.).
A 59-year old female with anthracycline-associated DCM progressed to end stage heart failure and received an LVAD as a bridge to transplant. Three months s/p LVAD placement, she developed abdominal pain and bright red blood per rectum (BRBPR). On admission, she was anemic and had an INR of 2.4. She subsequently developed intracranial hemorrhage and goals of care were adjusted to comfort measures only. Testing at this time showed reduced vWF activity. The autopsy showed the following findings. What was the most likely cause of death?Thank you to Dr. Michael Seidman for sharing this case.
Click here for the answer.
Acquired von Willebrand deficiency (vWD) in the setting of a ventricular assist device (VAD)
A 62-year old male with coronary artery disease (CAD) status post coronary artery bypass grafting (CABG) progressed to end-stage heart failure and received a transplant. The explanted heart showed the following findings. What was the unexpected diagnosis?Thank you to Dr. Michael Seidman for sharing this case.
Click here for the answer.
Hypertrophic Cardiomyopathy
A 2 year old with a complex medical history developed hypertrophic cardiomyopathy with left ventricular outflow tract obstruction. She underwent septal myectomy. What is the unusual cell type pointed to by the arrows?
Click here for the answer.
Interstitial-like cells of Cahal AKA Telocytes with swollen endoplasmic reticulum
A 61 year old woman underwent an endomyocardial biopsy for heart failure. She has a history of a meningioma and inflammatory arthritis. She is taking hydroxychloroquine daily.
Click here for the answer.
Myocardial lipid vacuolization
A 40 year old woman underwent a heart transplantation due to advanced heart failure. This process was found on her aorta.
Click here for the answer.
Sarcoidosis
A 42 year old man with a two year history of chronic myelomonocytic leukemia (CMML) was admitted for shortness of breath, night sweats and weight loss. After a long hospital stay, in which he continued to deteriorate, he expired and an autopsy was performed. What disease was unexpectedly found in his heart?
Click here for the answer.
Rosai-Dorfman Disease
A 63 year old man with CAD and prior MI, DCM, placement of a pacemaker/AICD and an ejection fraction of 15-20% presented to the hospital with weakness and dyspnea on exertion. He was found to be have a large pericardial effusion and cardiac tamponade physiology. An attempt was made to correct this problem but a complication arose and shortly afterwards the patient became unresponsive and died despite resucitiative efforts. What does the autopsy suggest happened?Thank you to Dr. Kevin Waters for sharing this case.
Click here for the answer.
Perforation of the right ventricle during pericardiocentesis.
Case #17 - A 58-year-old HIV+, HCV+ man had interesting histologic findings in his heart at autopsy.
A 58 year old HIV+, HCV+ man presented to the hospital with fever, chills and urgent diarrhea. He developed septic shock and multiple complications leading to his demise one week later. What process caused the histologic findings found in his heart at autopsy?Thank you to Dr. Doreen Nyugen for sharing this case.
Click here for the answer.
Thrombotic thrombocytopenic purpura (TTP) with occlusive microangiopathy.
A 65 year old man presented to the hospital after having an acute stroke and hwas found to have a left atrial mass on transesophageal echocardiogram (TEE).Thank you to Dr. Doreen Nyugen for sharing this case.
Click here for the answer.
Myxoma
A 31 year old woman came for routine endomyocardial biopsy seven years after heart transplantation. Her explanted heart demonstrated a chronic active myocarditis with focal giant cells. Two months prior to biopsy she was diagnosed with PTLD (Diffuse large B-cell lymphoma) in a lymph node, resulting in a decrease in her immunosuppresion. She had not begun definitive treatment for the PTLD yet.
Click here for the answer.
Recurrent giant cell myocarditis.
A 49 year old woman with Noonan Syndrome developed severe mitral valve regurgitation. During mitral valve repair the atrial appendage was also removed. This lesion was found at that time.
Click here for the answer.
Mesothelial incidental cardiac excrescence (MICE)
A 26 5/7 week old female fetus had in utero demise. At autopsy the only notable findings were accelerated placental maturation and this heart finding.
Click here for the answer.
Parietal pericardial defect with apical strangulation
A 35 year old woman has a mass in the IVC adjacent to the right atrium removed.
Click here for the answer.
Organizing thrombus
A 60 year old man underwent removal of his ascending aorta.
Click here for the answer.
High grade pleomorphic sarcoma of the aorta.
A 42 year old woman was admitted for a urinary tract infection and a positive blood culture for bacteria. After discharge, she was readmitted for severe aortic insufficiency requiring an aortic valve replacement. The specimen showed endocarditis (image 5). What else was unusual about this valve?
Click here for the answer.
Benign adipose infiltration. This was described in Pantanowitz L and Jiang L. Fatty infiltration of the aortic valve. Int J Cardiol 2009, 134:e59
A 60 year old woman underwent cardiac transplantation. The images are from a follow up surveillance biopsy.
Click here for the answer.
Deep and exuberant Quilty lesions
Case #8 - A 57-year-old man underwent cardiac transplantation for idiopathic dilated cardiomyopathy.
A 57 year old male underwent cardiac transplantation for idiopathic dilated cardiomyopathy. What cell type is the arrow pointing to?
Click here for the answer.
Basophilic degeneration.
A 50-year-old Afro-Carribean female presented with severe aortic regurgitation, aortic root aneurysm and cardiac decompensation. She refused surgical aortic repair. A CT scan showed occlusion of her left carotid artery and partial to severe stenosis of several other large arteries. A diagnosis was made and she was put on medications. Six months later, she redeveloped severe pulmonary edema and she finally agreed to aortic repair. Her dilated aortic root and aortic valve were resected. The valve was modestly thickened and unremarkable.
Click here for the answer.
Treated Takayasu Arteritis.
A 54 year old Caucasian female presented with a history of seasonal allergies, sinusitis, a spreading burning sensation in her legs with recent loss of balance, weight loss, and lower extremity edema. Laboratory values included an M-spike of 1.1 gm/dl, a CRP of 37.8 and a peripheral hypereosinophilia of 67%. An endomyocardial biopsy was performed.
Click here for the answer.
Eosinophilic myocarditis secondary to Churg-Strauss Syndrome.
An 83 year old Caucasian male underwent aortic valve replacement. This additional tissue was resected during that procedure.
Click here for the answer.
Foreign body giant cell reaction to atrial amyloid.
A 71 year old Caucasian female has a recent diagnosis of heart failure with possible restrictive physiology. She has a history of atrial fibrillation, diabetes, hyperlipidemia and hypertension. Her mother is alive and well in her 90s and her father died in his 40s of a heart attack. Five of six siblings are alive and without heart disease. She takes glyburide, simvastatin, metoprolol, aspirin, nifedipine, spironolactone and bumetanide. An endomyocardial biopsy was performed.Thank you to Dr. Charles Steenbergen for sharing this case.
Click here for the answer.
Fabry Disease.
A 67 year old female has right sided valvular heart disease. She has a history of prior abdominal surgery for a mass. A thickened pulmonic valve is removed.Thank you to Dr. Alex Chang for sharing this case.
Click here for the answer.
Carcinoid valve disease.
A 46 year old man has a two year history of hypertension and pulmonary embolism. He presented to the hospital with chest pain and dyspnea. Imaging showed an obstruction of the pulmonary artery. Two attempts at biopsying the obstruction were unsuccessful and the patient’s condition worsened, requiring intubation and finally support was withdrawn. An autopsy was performed. The proximal pulmonary artery was thickened to 3cm with a shaggy and irregular luminal surface.Thank you to Dr. Matthew Tilson for sharing this case.
Click here for the answer.
Pulmonary Artery Sarcoma.
A 27 year old man presents with a one week history of dyspnea. He has no significant past medical history. On admission his ejection fraction (EF) is 25%. An endomyocardial biopsy is performed.
Click here for the answer.
Giant cell myocarditis.